A few years ago I visited a storefront building called InSite – the first supervised injection facility in North America. There, I saw first hand that, paradoxically, providing a safe place to take illicit drugs can be a key component to treating addiction.
Located in Vancouver’s East Hastings neighborhood, the building was clean and the environment felt safe; I immediately noticed the rapport between the staff and the clients, who were mostly injection drug users.
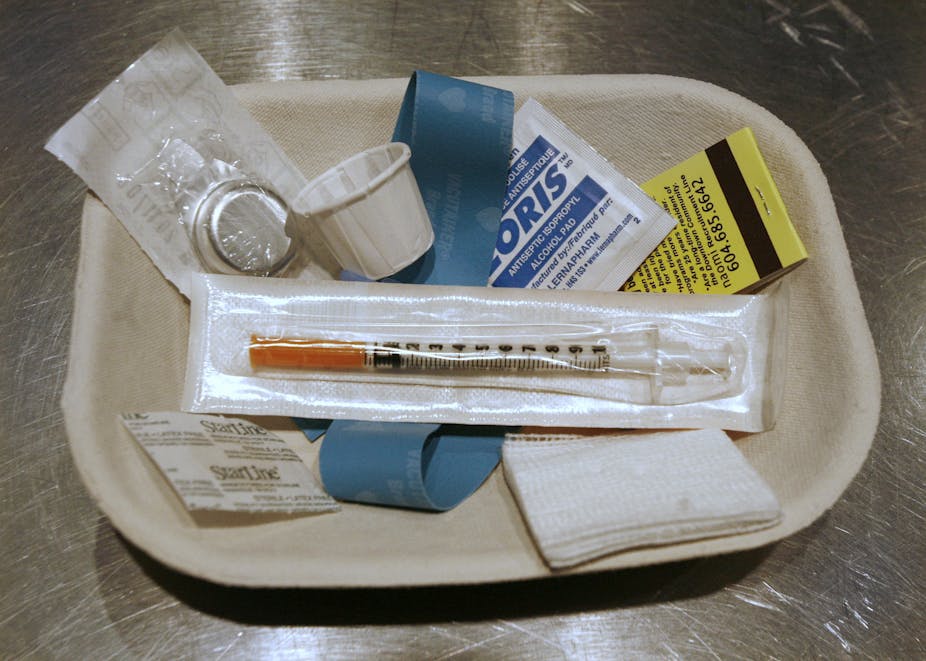
Clients arrived with what they were bringing to inject (usually heroin or cocaine) and gave their names to a staff member. The staffer then logged this information before the clients went upstairs to the injection stalls, where syringes and other paraphernalia were available.
At one point, I heard a siren and saw an ambulance pull up across the street from the facility. The staffer and I looked out the front window as two first responders ran up the steps of a dilapidated building and returned carrying an unconscious woman on a stretcher. As they put her in the back of the ambulance, the staffer explained that the building was a shooting gallery – a place where drug users rent rooms to inject together.
“She should have come here,” she said. “We have a nurse on staff.”
“And it would have saved the city the costs of the emergency response,” I added, watching the young woman leave the ambulance and return to the building.
An emergency ambulance costs about $1,000 per trip, on average – and much more if any medical supplies are used. Taxpayers absorb this cost for the uninsured.
Lowering public health costs is just one of the benefits of supervised injection facilities (SIFs); and with the current epidemic of street level drug use, there’s no better time to open SIFs in cities across America. Yet despite an overwhelming body of evidence that favors the implementation of SIFs – and the fact that SIFs have been successfully operating in Europe and Canada for years – no legal SIFs are currently open in the United States.
The public benefits of SIFs
Why are American policymakers so reluctant to establish SIFs?
It could be because SIFs offer users drug paraphernalia, like clean needles, along with a medically trained, emergency response staff. For some Americans, this might sound like a handout; for others it’s implicit support of drug use.
Nonetheless, there are a number of noted public benefits to SIFs.
The facilities can alleviate the financial burdens of the state (and taxpayer) by decreasing public health costs for medical care and emergency responses, while lowering criminal prosecution and incarceration costs. In the US, on average, per capita prison costs are $100. SIFs lower these costs by decreasing neighborhood crime and public drug use.

SIFs could also lower both emergency and long-term health care costs. Lifetime treatment costs of HIV infection is about $380,000 per infection. Studies consistently find that SIFs reduce the risk of HIV infections and other other health care expenses. For example, a person who overdoses on the street is ten times more likely to stay overnight in a hospital than one who overdoses in a SIF – saving public taxpayers $1,700.
From a public health perspective, SIFs provide a clean place to inject drugs – which reduces the spread of infectious diseases like HIV, AIDS and hepatitis C. Furthermore, wherever there are street drug users, an SIF makes the area safer by diminishing open drug use. It also curtails drug litter, such as drug bags, dirty cotton and used needles. Finally, they’ve been shown to reduce overdose deaths.
While SIFs – along with other harm-reduction approaches – focus on the health of drug users, there’s another important benefit to the facilities: they can increase the drug users’ social capital. Addiction is, above all, a social problem. And a better understanding of social causes would further build the case for these much-needed facilities.
Social roots of addiction
Humans are social creatures; most feel the need to belong to a group or community.
A little over three years ago, journalist Johann Hari traveled the world to investigate the universal causes of drug addiction. Talking with hundreds of people in places ranging from Brooklyn to Portugal, he found that drugs aren’t the drivers of addiction – isolation is. Yet our society often cuts off addicts from others, either by incarcerating them or socially segregating them in addiction treatment programs. And we have known for a long time that isolating addicts doesn’t make them stop using drugs.
Scientific research seems to support this.
Social scientist Bruce Alexander found that when rats were isolated in cages they self-administered morphine until they were addicted, but rats housed with other rats did not. He took this experiment further by putting the caged rats back into their natural habitat with other rats – and observed that they stopped using the drugs.
Another study using monkeys made a similar discovery. Whereas both dominant and subordinate male monkeys became addicted to cocaine when caged separately, after being housed with females only subordinate monkeys continued to self-administer cocaine.
These studies show that when it comes to addiction, social environment can have a stronger influence than brain chemistry. When I asked someone involved in the monkey study why we don’t use social remedies for drug problems, he said taking a pill is easier.
Social bonds increase social capital
Social bonding is one reason the 12-step model used by Alcohol Anonymous (AA) and other recovery groups is so popular. In these groups, recovering addicts form strong bonds with other recovering addicts, which facilitates their own recovery process. However, while this model works for a time, studies have shown that recovering addicts need to be engaged in a wider community, beyond AA. To become functioning members of society, they need to increase their social capital.
Social capital refers to the connections individuals form that give them the resources to live happy, healthy, fulfilled lives. As political scientist Robert Putnam explains in his groundbreaking 2000 book Bowling Alone, when we become disconnected from family and friends and feel isolated from society, our social capital is depleted. On the other hand, building social capital is a way to promote healthy citizens and a thriving community.
We’ve come a long way from thinking about addiction as a moral failure, but it’s important to also look beyond the notion that addiction is only a psychological disorder or brain disease.
As Johann Hari writes, “the opposite of addiction is not sobriety. It is human connection.”

A uniquely American SIF
Not all drug users become street addicts. Some are socially integrated, but these aren’t the ones we segregate. It’s drug injectors – especially the street injectors – who are marginalized and disenfranchised. And jailing them only increases their isolation. It’s important to give these users the opportunity to become engaged in community activities.
Historians have long recognized the distinctive American characteristic that blends rugged individualism with civic engagement and community involvement. An American version of a SIF can be much more than a place that simply provides safe and clean injection facilities. It also can offer social initiatives; it can act as a community that reduces social isolation and increases social capital.
Studies have shown that we form new relationships by engaging in new social networks. In a Decatur, Georgia drug court treatment program, I used social activities to connect individuals to the local community. Within weeks they were forming new social networks and displaying healthy social habits. One young man who attended slam poetry readings started writing poetry and reading his poems before a coffeehouse audience. Another recalled his own social transformation.
“Being a felon means that I’m in a separate entity in society,” he explained, “but now I have the opportunity to build relationships.”
Linking addicted drug users to new social networks – other than addicts or recovering addicts – provides new opportunities for work, leisure, and friendship. A socially-focused SIF can give drug users better ideas and resources for how to spend their time participating in group activities.

The time is ripe for change
In the last year, governors of the states hit hardest by the opiate epidemic have begun speaking out. The governor of Vermont made it a central part of his State of the State speech last year. Meanwhile, Charlie Baker, the new governor of Massachusetts – where there has been a 46 percent increase in opiate deaths since 2012 – has made this issue one of his top priorities. His 16 member Opioid Addiction Working Group is tasked with engaging with communities and developing evidence-based strategies to combat addiction. The time is ripe for state legislation supporting SIFs that not only responds to combating addiction, but also offers a path to healthy community engagement.

After more than ten years of experimenting with SIFs in other countries, what additional evidence do we need? Beyond reducing health care and social services costs, a SIF facilitates drug treatment, and can provide bridges to new social networks so that those most ravaged by addiction can become productive members of society.
This is the third in a series of three articles on alternative strategies to treat addiction. To read the first in the series, click here. To read the second article, click here.