This edition of the infohep.org bulletin is devoted to news from The Liver Meeting, organised by the American Association for the Study of Liver Diseases (AASLD), which took place in San Francisco, USA, from 13-17 November 2015.
Having trouble reading this email? View it in your browser
| |
November 2015 | |
News from The Liver Meeting 2015, San FranciscoAccess to hepatitis C treatment in the United States: doctors and federal government urge wider accessThe American Association for the Study of Liver Diseases (AASLD) warned at its annual Liver Meeting that too many people with hepatitis C virus (HCV) are being denied treatment by insurance companies without medical evidence to justify their decisions. A growing body of research underlines the importance of timely treatment, showing that the benefits of curing hepatitis C are greater if it is cured before advanced liver disease develops. Recent guidance from the AASLD recommended earlier treatment for hepatitis C, before progression to advanced liver damage. “HCV treatment that leads to a cure is the only evidence-based intervention to prevent liver disease progression,” AASLD said in a statement issued at the conference. “A significant proportion of people living with HCV who have no or mild fibrosis (commonly described as F0-F2) will progress to cirrhosis in the absence of treatment. Currently, there is no way to predict who will develop advanced liver disease.” The federal agency responsible for setting standards for the Medicaid insurance programme for people on low incomes (Centers for Medicare & Medicaid Services) has written to state Medicaid programmes stating that they are expected to cover new interferon-free antiviral therapies for hepatitis C without undue restrictions. It has also written to the pharmaceutical companies that make these drugs asking about purchasing arrangements to ensure wider access. A survey of hepatitis C prescriptions through one pharmacy chain in four US states presented at The Liver Meeting showed that almost half of Medicaid-insured patients had their prescriptions for hepatitis C treatment turned down, and in an alarming number of cases the state Medicaid office did not bother to send a letter to say that the treatment would not be funded, leaving patients waiting and unable to appeal. The study found that one in six people with private insurance or Medicare insurance for senior citizens and people with disabilities were denied reimbursement. Long-term outcomes after hepatitis C treatment: liver cancer
The burden of liver cancer and cirrhosis caused by hepatitis C is likely to continue to grow in the United States despite curative treatment for hepatitis C, and people who have cirrhosis at the time they are cured of hepatitis C will require long-term monitoring for liver cancer, studies presented at The Liver Meeting showed. A study of the Veterans Affairs Hospitals database looked at how being cured of hepatitis C had affected the risk of developing liver cancer. The study found being cured reduced the risk of liver cancer by 64%, but did not eliminate it. People who had cirrhosis at the time they were cured were around four and a half times more likely to develop liver cancer compared to those without cirrhosis, as were people over 65 when compared to under-55s. A second study used trends in the Veterans Affairs population to project what will happen in the United States. The investigators found that the incidence of both cirrhosis and hepatocellular carcinoma are likely to continue rising in the United States until 2021, even taking into account the impact of treatment. Investigators of a third study concluded that the size of the US population of people with hepatitis C who have cirrhosis has increased from approximately 170,000 in the period 1988-1994 to 370,000 in the period 2007-2012. The investigators warned that due to the lack of symptoms in earlier stages of cirrhosis, many people may be unaware that they have hepatitis and advanced liver disease, and doctors should be particularly alert to the risk of cirrhosis in people with hepatitis C who are older, those with diabetes and those with high body mass index. These findings emphasise the importance of early diagnosis and early treatment for reducing the lifetime risk of liver cancer for individuals, and for reducing the overall burden of ill health related to hepatitis C. Long-term outcomes after hepatitis C treatment: reversal of liver damage
People who do not receive treatment for hepatitis C until they have developed advanced fibrosis or cirrhosis want to know whether treatment is able to reverse liver damage. Long-term follow-up of people cured of hepatitis C is needed to answer this question, and to predict who might be more likely to experience improvement. A study of 100 people with cirrhosis cured of hepatitis C with direct-acting antiviral treatment at one hospital in the United States found that 69% of people with advanced fibrosis and 55% with cirrhosis experienced an improvement in the health of their liver as measured by Fibroscan (using transient elastography, similar to an ultrasound). Overall, only 6% of people experienced a worsening of liver damage after being cured of hepatitis C. The median time to improvement was 2.5 years for people with advanced fibrosis and 3.0 years for those with cirrhosis at baseline, indicating that those with less severe liver injury improved faster. The researchers identified few factors in this study that predicted fibrosis improvement or worsening. Diabetes and varices were associated with a lower likelihood of fibrosis improvement. Hepatitis C treatment for people who inject drugs
Hepatitis C virus (HCV) is easily transmitted through sharing drug injection equipment, and current and former injecting drug users have high rates of infection (50% to 80% in some studies). But many providers and insurers still consider people who inject drugs to be poor candidates for treatment and active drug users have been excluded from most trials of new direct-acting antiviral agents. Merck's grazoprevir/elbasvir co-formulation cured hepatitis C infection in 92% of people who inject drugs who were receiving opioid substitution therapy in the C-EDGE CO-STAR study. Participants maintained good adherence and had a high cure rate even though many continued to use illicit drugs. "The safety and high efficacy convincingly demonstrate the benefits of treating HCV within this population," said Dr Greg Dore of the Kirby Institute at the University of New South Wales, Australia. "Such evidence should enhance access to new HCV therapies, including removal of restrictions to access in many settings based on illicit drug use. This study offers reassurance to providers who are concerned that patients who actively use illicit drugs will not be adherent to their chronic HCV treatment." Treatment for genotype 3
Genotype 3 infection is associated with an increased risk of fibrosis progression and liver cancer (hepatocellular carcinoma) compared to other genotypes, making affordable and effective treatment options for people with HCV genotype 3 an important unmet need. Genotype 3 hepatitis C infection is more difficult to cure than other genotypes of hepatitis C, requiring a longer course of treatment with most regimens. The only currently approved 12-week interferon-free regimen for treatment of genotype 3 consists of daclatasvir (Daklinza) and sofosbuvir (Sovaldi). Almost 30% of worldwide hepatitis C infections are estimated to be genotype 3, with a particular concentration in the Indian sub-continent and among populations of South Asian origin living elsewhere. Genotype 3 is also widespread in the Russian Federation, Scandinavia, Thailand, Brazil and Australia. Findings presented at The Liver Meeting showed that the combination of daclatasvir (Daklinza) and sofosbuvir is highly effective in the treatment of genotype 3 infection. The ALLY-3+ trial, a post-marketing study in people with advanced fibrosis (F3 stage) or compensated cirrhosis, showed that the combination of daclatasvir, sofosbuvir and ribavirin cured 88% of people treated for 12 weeks and 92% of people treated for 16 weeks. Reports from two compassionate access programmes, in Germany and France, showed good cure rates in people with compensated cirrhosis and in the small groups of people with decompensated cirrhosis treated through these compassionate access programmes. The German cohort study found no difference in response between those who received ribavirin and those who did not. Several studies presented at The Liver Meeting showed that new experimental regimens also achieved very high cure rates in people with genotype 3 infection, without the use of ribavirin. AbbVie presented results of a phase 2 study of a new two-drug interferon-free regimen. ABT-493 is an HCV NS3/4A protease inhibitor active against all genotypes of hepatitis C. ABT-530 is an NS5A inhibitor also active against all genotypes of HCV. Both agents are active against common variants that confer resistance to first-generation agents of their classes. The study recruited previously untreated people or previous null responders to pegylated interferon and ribavirin, with no evidence of cirrhosis. The combination cured 93 to 97% of people with genotype 3 hepatitis C infection after a 12-week course of treatment. Gilead presented results from the 12-week ASTRAL-3 study. A co-formulation of sofosbuvir (Sovaldi) and the pan-genotypic HCV NS5A inhibitor velpatasvir produced sustained response in 95% of those with harder-to-treat genotype 3 in this study. Around one quarter of participants were treatment-experienced and 30% had cirrhosis. Gilead also presented results of a study in which a third agent, the protease inhibitor vedroprevir, was added to sofosbuvir and velpatasvir. Treatment with this regimen lasted 6 or 8 weeks. In the genotype 3 group in this phase 2 study, the SVR12 rate was 83% in the cohort of treatment-naïve people with cirrhosis who were treated for 6 weeks. In the treatment-experienced cohort of people with cirrhosis treated for 8 weeks, 100% achieved SVR12. Related links
New drugs: pan-genotypic treatment combinationsPan-genotypic treatment for hepatitis C refers to a combination of drugs which is effective against all genotypes of hepatitis C. Pan-genotypic treatment combinations might improve access to treatment in several ways. The availability of pan-genotypic treatment would eliminate the need for expensive genotype testing prior to treatment, reducing the overall cost of treatment. Pan-genotypic treatment would also simplify the provision of treatment in countries where several different genotypes are widespread in the population of people living with hepatitis C. One combination could be prescribed for most people with hepatitis C, simplifying drug supply and procurement. Treating a larger number of people with the same combination might make it easier to negotiate lower prices. New pan-genotypic treatment combinations are being developed by several companies. The Liver Meeting heard findings on several of these combinations, the first of which could receive marketing approval in the first half of 2016. Gilead presented results of the four ASTRAL studies showing that the combination of sofosbuvir and the pan-genotypic HCV NS5A inhibitor velpatasvir produced sustained response in 99% of people with hepatitis C virus genotypes 1, 2, 4, 5 and 6, and 95% of those with harder-to-treat genotype 3. The four large studies treated 1797 people, including 267 people in the ASTRAL-4 study of treatment in people with decompensated cirrhosis. The ASTRAL-4 study found SVR12 rates of 83% and 86% for people treated with sofosbuvir/velpatasvir for 12 or 24 weeks, respectively, rising to 94% for those who added ribavirin. The effect of adding ribavirin was most pronounced in people with genotype 3 who had decompensated cirrhosis: only 50% achieved SVR12 if they received sofosbuvir/velpatasvir without ribavirin, while 85% cleared the virus when ribavirin was added to their treatment. This co-formulated combination has been submitted for marketing approval in the United States and the European Union and is likely to be approved in the first half of 2016. AbbVie presented results of phase 2 studies of its pan-genotypic combination of ABT-493, an HCV NS3/4A protease inhibitor active against all genotypes of hepatitis C, and ABT-530, an NS5A inhibitor also active against all genotypes of HCV. The SURVEYOR-1 study tested the combination in people with genotype 1, and the SURVEYOR-2 study in people with genotypes 2 and 3. The studies compared various doses, with or without ribavirin. In SURVEYOR-1 the combination cured 97 to 100% of people without cirrhosis. In SURVEYOR-2, the combination cured 96 to 100% of people with genotype 2 infection and 93 to 97% of people with genotype 3. In all cases, participants received 12 weeks of treatment. Phase III studies are about to begin, and studies will also test the efficacy of an 8-week treatment course. Related links
Daclatasvir licensed to Medicines Patent Pool
The Medicines Patent Pool (MPP) this week announced its first licence for a hepatitis C medicine, signing an agreement with Bristol-Myers Squibb for daclatasvir, a direct-acting antiviral that is proven to help cure multiple genotypes of the hepatitis C virus. The royalty-free licence will enable generic manufacture of daclatasvir for sale in 112 low- and middle-income countries (LMICs), 76 of which are World Bank classified middle-income nations. Nearly two-thirds of all people living with hepatitis C in LMICs reside in the territory covered by this agreement. Importantly, the licence allows generic manufacturers to develop fixed-dose combinations with other direct-acting antivirals to create powerful pan-genotypic regimens that offer the potential to treat all of the six major genotypes of HCV. “The licence comes shortly after the MPP announced its mandate expansion into the area of hepatitis C and on the heels of a six-month dialogue with patient groups, civil society and other stakeholders on best approaches to improving access to new curative HCV solutions,” said Greg Perry, Executive Director of the MPP. “Thus, we believe the licence takes into consideration the concerns of patient advocates who have been campaigning for some time for new life-saving innovations such as daclatasvir to reach more people quickly.” Sofosbuvir and bradycardia
French doctors have warned that sofosbuvir treatment for hepatitis C may be associated with the slowing of the heartbeat in rare cases. In a letter to the New England Journal of Medicine they have reported three cases of “severe” bradyarrhythmia, also known as bradycardia. Bradycardia had already been identified as a potential risk in people taking sofosbuvir with amiodarone, a drug used to treat cardiac arrhythmia. The French case reports are the first to describe episodes of bradycardia in people taking sofosbuvir without amiodarone. The authors say that, before prescribing sofosbuvir, doctors should look at other risk factors for bradyarrhythmia, and consider monitoring heart rhythm during the early weeks of treatment (all the reported episodes occurred within ten days of starting treatment). World Hepatitis Summit report and resources
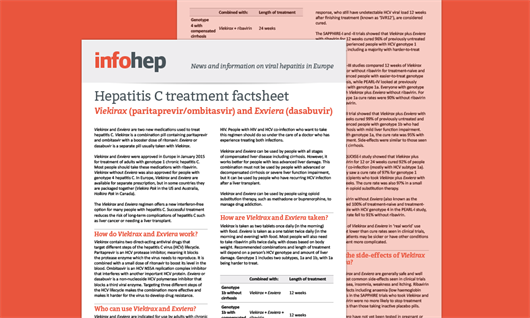
A report on the World Hepatitis Summit authored by NAM and presentations and webcasts from the World Hepatitis Summit are now available. New hepatitis C treatment factsheet
We have recently published a factsheet on two new medications used to treat hepatitis C: Viekirax (paritaprevir/ombitasvir/ritonavir) and Exviera (dasabuvir). This is an addition to our six other hepatitis C treatment factsheets. The factsheets focus on direct-acting antiviral drugs and give an overview of how they work, who can use them, how they are taken, what trial results tell us about how effective they are, known side-effects and drug interactions. The factsheets are available to read online, and are also designed to be printed and shared. Related linksIs this your copy of the infohep news bulletin?
Is this your copy of the infohep news bulletin, or did you receive it from a friend or colleague, or find it online? You can sign up to receive this monthly email bulletin, free of charge, on our website, where you can also find an archive of all the infohep news bulletins. | |
 Latest treatment news and information for patient advocates and people working in hepatitis in Europe. For more details, please contact: To unsubscribe please click here Privacy Policy |



Connect with infohep on Facebook: Keep up to date with all the latest news and developments.
Follow infohep on Twitter for links to news stories and updates from infohep.org. Follow us at www.twitter.com/infohep.
Follow all the infohep news by subscribing to our RSS feeds.